Research
Increasing Inpatient Coder Productivity by Optimizing CAC
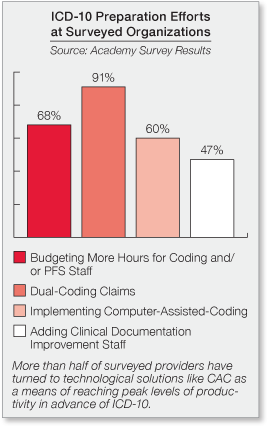
As healthcare organizations continue searching for ways to increase coder productivity and accuracy as a means of mitigating the impact of ICD-10, many providers have turned toward solutions such as computer-assisted coding (CAC). In order to achieve the full benefits of this technology, however, it is important for leaders to continually explore avenues for ensuring system logic best supports staff and coding processes—helping to promote clean claims and reduce denials.
To this end, The Academy recently spoke with the director of coding at a 12-hospital health system based in the Midwest. By promoting open communication with its CAC vendor and encouraging coders to incorporate the technology into their daily workflows, this organization has been able to increase coder productivity and raise its case mix index (CMI).
 Maximizing Vendor Partnerships
Maximizing Vendor Partnerships
The health system implemented CAC for its inpatient services in 2013 and quickly thereafter rolled it into the outpatient realm. This technology is paired with an external solution for ancillary areas (e.g.